SEI provides patients with modern
choices
by
Heather WoolwinePublic Relations
Only a few things are as frightening as losing one of the five senses granted most people at birth. For patients suffering from age-related macular degeneration (AMD), blurred, spotty or reduced vision indicates a future of total darkness if they do not stop the curtain from falling over their sight.
Meanwhile, MUSC’s Storm Eye Institute (SEI) is shedding light and expanding its service for AMD patients. As the only place in the Charleston area where patients can choose from every available AMD treatment option, SEI offers all available AMD treatments on campus, at its new North Charleston office, and in Mount Pleasant.
“Since we are able to offer all available treatment options, we can focus on the individual needs of each patient, not only what our treatment limitations are,” said Esther Bowie, M.D., ophthalmologist and AMD specialist.
The North Charleston and Mount Pleasant offices function much like private practices, but patients have access to the extensive network of eye care specialists at SEI. “We’re a comprehensive ophthalmology clinic that can provide our patients with quick evaluations and access to other experts within the MUSC system, if needed,” Bowie explained. “We anticipate an increase in the number of patients with macular degeneration because of the increase in an aging population.”
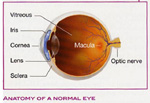 AMD
is divided into two types—dry and wet. The most common, with 90 percent
of patients presenting with AMD, is the dry type. Dry AMD is marked by
a slow, progressive loss of central vision and difficulty adjusting to
dark settings.
AMD
is divided into two types—dry and wet. The most common, with 90 percent
of patients presenting with AMD, is the dry type. Dry AMD is marked by
a slow, progressive loss of central vision and difficulty adjusting to
dark settings.Wet AMD, for the remaining 10 percent of people with this condition, is marked by abnormal blood vessels growing beneath the retina that bleed and leak fluid into the eye. The result for the individual is viewing distorted lines and a sudden decline in central vision that, if left untreated, can render a person blind.
Given the two types, wet AMD is the most debilitating, and until now has been the most difficult to treat. Since the end of June, MUSC has been using a new anti-vascular endothelial growth factor (anti-VEGF) called Lucentis to offer AMD patients one of the best options for stabilizing and improving vision loss.
“I’ve had one patient who went from barely being able to count fingers that were held up in front of her to watching TV,” Bowie said. “Previous treatments did not provide such a possibility for dramatic change in vision after the onset of the wet type of macular degeneration.”
A brief history of AMD treatment
 For
the 1.75 million Americans with AMD, bookshelves don’t look straight,
street signs are blurred, or spots in central vision make even the most
basic of daily tasks difficult to undertake. These individuals suffer
from the leading cause of vision loss in people older than 50, and
often have risk factors that include: age 50 years or older, a family
history of AMD, typically female and Caucasian, a history of smoking,
and a medical history that includes uncontrolled hypertension, high
cholesterol and obesity.
For
the 1.75 million Americans with AMD, bookshelves don’t look straight,
street signs are blurred, or spots in central vision make even the most
basic of daily tasks difficult to undertake. These individuals suffer
from the leading cause of vision loss in people older than 50, and
often have risk factors that include: age 50 years or older, a family
history of AMD, typically female and Caucasian, a history of smoking,
and a medical history that includes uncontrolled hypertension, high
cholesterol and obesity.Prior to 1981, no treatment existed for wet AMD. That year, thermal laser technology was introduced to help patients with wet AMD stabilize their vision loss by essentially cauterizing leaky blood vessels in the eye. Eighteen years later, photodynamic therapy (PDT) was introduced. PDT utilizes a photoactive drug called Verteporfin that is activated by a laser, which in turn leads to vascular thrombosis in the treated area. In other words, the treatment option was much better for many patients at preventing further vision loss but did little in the majority of patients to improve upon vision loss.
In 2001, dietary supplements called antioxidants found a niche in the care of patients with the dry type. A breakthrough came in 2004 with the implementation of anti-VEGF drug therapy.
Anti-VEGF agents decrease the growth of abnormal blood vessels and decrease the amount of fluid in the eye. The first drug on the market was Macugen. Patients undergoing this therapy must have an intraocular injection every six weeks. Seventy percent of patients maintained their vision and 6 percent treated saw an improvement in their vision. This was a huge accomplishment in terms of treating wet AMD because of the significant improvement in vision for some patients.
Last year, Bowie and her colleagues joined a handful of practitioners around the country who began to use Avastin, a drug made for patients with colon cancer, to help treat wet AMD. Preliminary results from intraocular injections using Avastin are promising, but it is still not approved by the FDA for wide-spread use.
In June of this year, Lucentis arrived as a cousin, of sorts, to Avastin. One of the issues in treating patients with Avastin was the size of the drug molecule; it was too large to pass through the retina on its own. With Lucentis, the molecule was refined to penetrate the retina completely. Patients in clinical trials with Lucentis showed an increase in vision for 30 percent to 40 percent of patients, and stabilized vision for 95 percent of patients who received injections every four weeks, offering by far the best results in stabilizing and improving vision for people with wet AMD.
Customized treatment
Every patient should understand that while these procedures have revolutionized care for wet AMD, they are not cures. Patients will have to be treated for wet AMD from diagnosis throughout the rest of their lives. However, what may begin as a monthly treatment could translate into treatment on an as-needed basis, depending on the patient. In addition to selecting the treatment most appropriate for them, patients monitor their vision with Amsler grids.
“At MUSC, patients have the option of letting treatment evolve, because each patient is different. One example is a patient of mine who began his treatment with Macugen, then he tried Avastin, now he uses Lucentis,” Bowie said.
Patients may decide to change treatment options based on their needs or because they may not respond as well to one type of treatment versus another.
Some side effects are associated with intraocular injections, but there is less than a one percent chance of developing those side effects. Negative side effects include endophthalmitis (infection), a retinal tear, retinal detachment, lens damage, and Avastin and Lucentis may cause increased risk of heart attack and stroke (though not statistically significant).
“We take all precautions to prevent any side effects from occurring, including antibiotics post-treatment, the use of sterile equipment and follow-up with the patient,” Bowie said.
In addition to offering the most comprehensive treatment for AMD in the Lowcountry, SEI also has an AMD support group. The group met for the first time in July and will meet again Oct. 16.
“Macular degeneration can be a very frightening condition for patients, so it's important and helpful to have patients reassure one another that there are other people who understand what they are going through,” Bowie said.
The group provides a forum for patient education, information about treatments and diagnosis, and discussion about issues AMD patients must deal with on a daily basis.
For information about the support group, contact Carolyn Cavanaugh at 792-4735.
To schedule an appointment, call 792-8100.
Friday, Oct. 13, 2006
Catalyst Online is published weekly,
updated
as needed and improved from time to time by the MUSC Office of Public
Relations
for the faculty, employees and students of the Medical University of
South
Carolina. Catalyst Online editor, Kim Draughn, can be reached at
792-4107
or by email, catalyst@musc.edu. Editorial copy can be submitted to
Catalyst
Online and to The Catalyst in print by fax, 792-6723, or by email to
catalyst@musc.edu. To place an ad in The Catalyst hardcopy, call Island
Publications at 849-1778, ext. 201.