|
|
|

|
Cardiac MRI shows how triathletes' hearts adapt
|
The changes
in the heart that occur in triathletes represent a unique adaptation of
the heart muscle to the specific training that is involved with
triathlons, that is markedly different from other sports disciplines,
according to Joseph Schoepf, M.D., a co-investigator in a study to be
published in the October issue of Radiology.
The multicenter study was led by researcher Michael Lell, M.D., and
colleagues at the University of Erlangen-Nuremberg in Germany. The
study’s findings are significant in that the results differ from
previous research in other types of elite athletes.
“The interesting findings point to specific and unique patterns that
were observed in triathletes,” said Schoepf, a professor of radiology
and medicine at MUSC. “These changes have not been observed with
cardiac MRI before, so it’s the first study that used MRI [magnetic
resonance imaging] to really look at those things.”
Most earlier studies focused on the effects of either resistance or
endurance training, but this study did both since participation in
triathlons relies on both components as far as long-term cardiac
adaptation is concerned, he said.
 The MUSC
cardiovascular imaging team, Dr. Joe Schoepf, from left, radiological
technologist Rob Finch, and Dr. Markus Weininger, with the Tesla
scanner. The MUSC
cardiovascular imaging team, Dr. Joe Schoepf, from left, radiological
technologist Rob Finch, and Dr. Markus Weininger, with the Tesla
scanner.
The researchers
enrolled a total of 26 male triathletes, ages ranging from 18 to 35,
with six or more years of continuous training, as well as 27 male
control subjects ages 20 to 34, who were recreationally active no more
than three hours per week. All 53 subjects were examined with a 1.5
Tesla scanner.
Findings showed that the human heart adapts to triathlon training by
developing greater muscle mass and wall thickness, as well as larger
left atria and larger right and left ventricles. Schoepf said it’s
important to understand the processes that are involved in the heart’s
adaptation to the physiologic stimuli of sports and pathologic stimuli,
such as hypertension. It also is important to recognize the heart
changes in high-performance athletes as a normal and desirable reaction
of the body so that they can be differentiated from pathologic
processes, such as hypertrophic cardiomyopathy, which is the number one
cause of sudden cardiac death in young athletes.
“The knowledge gained through this study helps us to recognize or
exclude disease in athletes who may experience symptoms such as
irregular heart rates, palpitations, or chest tightness while
exercising,” Schoepf said.
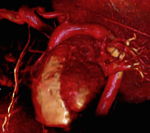 A high-resolution,
non-invasive magnetic resonance imaging study of the heart displayed as
a three-dimensional reconstruction. A high-resolution,
non-invasive magnetic resonance imaging study of the heart displayed as
a three-dimensional reconstruction.
The study found
the triathletes had lower blood pressure and resting heart rates 17
percent lower than those in the control group, which was expected.
“These are common and well-recognized effects of sports training in
physiology,” Schoepf said. But the significantly higher left
ventricular and end-diastolic volumes in triathletes were both
significant and unexpected.
As for future work, Schoepf said it would be interesting to use MRI to
look at specific adaptive changes in other kinds of athletes, and to
examine the differences between healthy triathletes and patients with a
condition such as hypertrophic cardiomyopathy.
Cardiac MRI is a precise non-invasive way researchers can assess the
heart muscle in disease states, which makes it a useful tool for
collaborative studies, he said.
“At MUSC we have the luxury of the most state-of-the-art imaging
equipment that is currently available for performing this kind of test
as well as an interdisciplinary team of physicians with unparalleled
experience in non-invasively imaging the heart.”
The cardiovascular imaging group at MUSC regularly hosts visiting
physicians from around the globe for training and research in advanced
cardiovascular imaging techniques, he said.
“Our international network is vast and forms the foundation for
exciting collaborations with research groups all over the world. The
current study is a product of this global outreach.”
Friday, Oct. 1, 2010
|
|
|