|
By
Dawn Brazell
Public Relations
Sometimes Michael Sweat,
Ph.D., has to eat goat. It's not a favorite part of the MUSC
researcher's job in Africa, but he understands why it's necessary.
"It's a big cultural thing
for them to have these big cookouts with a big goat they've
slaughtered, and you're the honored guest so you have to eat these big
chunks of goat they're giving you."
Sweat grimaces, but then
grins. His willingness to respect the local customs is one reason he
and a team of researchers have had success in an ambitious, eight-year
HIV study that was recently published in Online First "The Lancet
Infectious Diseases." Interim findings from the National Institute in
Mental Health's (NIMH) Project Accept combined data from 10 communities
in Tanzania, eight in Zimbabwe and 14 in Thailand.
 Dr. Michael
Sweat holds up a Tanzania map where he oversaw a research team. Dr. Michael
Sweat holds up a Tanzania map where he oversaw a research team.
Thrilled the study shows
the value of community-based voluntary counseling and testing (CBVCT),
Sweat sees this as another step in changing social policy to put a dent
in the tide of the AIDS epidemic that just keeps going. With an
estimated 2.8 million new HIV infections in sub-Saharan Africa in the
past year alone, 24.7 million Africans are now living with the virus.
 Dr. Michael Sweat gets water using
a hand pump. This is the type of setting researchers sought out to
provide intervention for local villagers. Dr. Michael Sweat gets water using
a hand pump. This is the type of setting researchers sought out to
provide intervention for local villagers.
"It's a big problem.
There's a huge mortality. There are a lot of orphans from AIDS. There
are a lot of widows and people affected. There are about 9 million
people in Africa who are infected and don't have access to treatment.
There's a big need to do something about it. Our intervention has a lot
of treatment implications."
The goal is to get people
to reduce risk-taking behavior and therefore slow down the transmission
of HIV, but also to get them on treatment because that's a life-saving
intervention, he said. Their study examined the impact of reaching out
to rural communities in creative ways through a four pronged approach
involved in CBVCT. They were:
- Doing mobile HIV
testing to reach isolated communities set up in highly visible sites,
such as the center of villages or water pumps, where villagers were
likely to congregate;
- Enlisting local
community support for greater "buy in" and encouraging fun ways to do
outreach, such as skits and community events;
- Performing
post-testing support to encourage people to disclose status and to
better serve the extensive psycho-social needs of those infected and;
- Using social
marketing techniques, such as feedback loops in the management system,
to constantly monitor the strengths and weakness of the program, and
make changes as you go. This strategy borrows techniques used by
companies such as Coca-Cola.
"You can go to any
developing country in the world and buy a Coke, and there's a reason
for that. These companies know how to do it. They know how to get
people excited about it. They know how to brand these products and make
sure the logistics are in place to get the commodities there. We
borrowed that model. If you can do that in this area, you can also do
it in health."
Interim findings
support what they did worked. 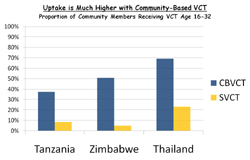
Sweat, who is
director of MUSC's Family Service Research Center in the Institute of Psychiatry, said he had a
Tanzanian local staff of 100 and eight vehicles. One of four U.S.
principal investigators on the multi-country study, Sweat leads the
Tanzania team. He and his group had to create maps of the Tanzanian
areas they served by driving around with GPS and manually recording
where every home was located. They did more than 9,000 interviews and
got blood samples using an exciting new technology that allows them to
see whether an infected person has a new infection or not—important
information in determining transmission patterns.
"This was like a
dream study. These are all people I've worked with for years," said
Sweat, whose impressive resume includes work with the Centers for
Disease Control and Prevention, Family Health International and 12
years at the Department of International Health at John Hopkins
University.
 This community outreach project
involved an educational skit about how women can pass the HIV virus to
their infants. This community outreach project
involved an educational skit about how women can pass the HIV virus to
their infants.
"It was one of
NIMH's biggest studies. It took a long time and a lot of effort, but it
was great. We had the best of the best. We have a statistics center in
Prague who handles a lot of our biostats. We have a data management
center in India that was fantastic. We have a lab at Johns Hopkins that
handles a lot of the laboratory work. It was cool."
There are 52,000
blood samples being shipped from five sites in four countries to
Baltimore for analysis, so in about a year, the group will be
publishing another paper analyzing if transmission rates have dropped.
"We hope it reduces
the number of new infections of HIV. If this were to do that, that
would mean this intervention could be replicated and could slow this
epidemic down. That would be so important. It would lead to a policy
change and people would start doing more door-to-door testing—this
mobile provision in rural areas."
Sweat said the way
they did mobilization created a positive energy about being tested. "It
became normative to get tested—everyone was doing it. A lot of people
felt safe doing it. But I also think putting it where people lived made
the difference. It's a very poor region and a lot of people have to
walk to get to the clinics. It can be a four-hour walk."
One of the goals of
the project was to destigmatize the process of getting tested, and
Sweat knows they were successful in challenging the concept that HIV
testing centers should be hidden away.
"We went in the
totally opposite direction and said we're not going to hide. We're
going right in the middle of the village next to where people get their
water or gather. We want people to visibly have to walk in the door and
be seen by other people. It made it safe for other people, and we got
huge numbers of people coming."
Bringing up Malcolm
Gladwell's book "The Tipping Point," Sweat said the study was not just
about doing "lots of testing" but about affecting cultural change
"It was the idea
that you change norms in the community—that if you get to a critical
mass to a certain tipping point that Gladwell writes about in his
book—where people are talking about it, then you'll have less
transmission from HIV."
It's news that the
United States can use, since research is showing the AIDS epidemic in
the United States is more concentrated among the poor, a factor that
has played out globally. Many of the big breakthroughs the field has
had were discovered by researchers doing work in developing countries.
"It is also notable that
since the rates of HIV infection are so high in many developing
countries, it is much easier to detect if they work there. This allows
us to benefit from this knowledge in the U.S."
Sweat likes how
international research can shed light on health disparities at home.
Having already submitted another grant proposal, Sweat said MUSC's
focus on globalization is impressive and that he has found it to be a
supportive environment. It probably means eating more goat in his
future.
For more
information:
Project Accept is the first
international randomized controlled Phase III trial to determine the
efficacy of a behavioral or social science intervention concerning the
incidence of HIV. The Project Accept website is http://www.cbvct.med.ucla.edu/.
For the full text version
of the study published in Online First in "The Lancet Infectious
Diseases," visit http://www.thelancet.com/journals/laninf/article/PIIS1473-3099(11)70060-3/fulltext.
Spotlight on Research
In the study,
communities in each setting were paired according to demographic
characteristics, and one of each pair was then randomized to receive
either standard, clinic-based voluntary counselling and testing SVCT
alone, or SVCT and community-based voluntary counselling and testing
(CBVCT).
 The researchers found that the
proportion of people receiving their first HIV test from the study was
higher in CBVCT communities than in SVCT communities in Tanzania (37
percent vs 9 percent), Zimbabwe (51 percent vs 5 percent), and Thailand
(69 percent vs 23 percent). The researchers found that the
proportion of people receiving their first HIV test from the study was
higher in CBVCT communities than in SVCT communities in Tanzania (37
percent vs 9 percent), Zimbabwe (51 percent vs 5 percent), and Thailand
(69 percent vs 23 percent).
Repeat
HIV testing in CBVCT communities increased to reach an average of 28
percent across the three countries.
|



 Dr. Michael
Sweat holds up a Tanzania map where he oversaw a research team.
Dr. Michael
Sweat holds up a Tanzania map where he oversaw a research team. Dr. Michael Sweat gets water using
a hand pump. This is the type of setting researchers sought out to
provide intervention for local villagers.
Dr. Michael Sweat gets water using
a hand pump. This is the type of setting researchers sought out to
provide intervention for local villagers.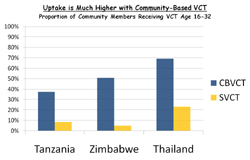
 This community outreach project
involved an educational skit about how women can pass the HIV virus to
their infants.
This community outreach project
involved an educational skit about how women can pass the HIV virus to
their infants. The researchers found that the
proportion of people receiving their first HIV test from the study was
higher in CBVCT communities than in SVCT communities in Tanzania (37
percent vs 9 percent), Zimbabwe (51 percent vs 5 percent), and Thailand
(69 percent vs 23 percent).
The researchers found that the
proportion of people receiving their first HIV test from the study was
higher in CBVCT communities than in SVCT communities in Tanzania (37
percent vs 9 percent), Zimbabwe (51 percent vs 5 percent), and Thailand
(69 percent vs 23 percent).